Screening for rare disease with next generation sequencing
Written by Celina Whalley on February 28th, 2024 | Reviewed by Sabahat Shamsuddin
How rare is rare?
To coin rare disease as ‘rare’ is a bit of a misnomer. Generally the definition of a rare disease, also known as ‘orphan disease’, is a medical condition affecting a small percentage of the population compared with other diseases.1 With this in mind, in the United States, a disease is considered rare if it affects fewer than 200,000 people at any given time. Similarly, within Europe, the definition extends to diseases that affect fewer than 1 in 2000 people.2,3
However, when looking at the collective prevalence the figures speak for themselves clearly emphasizing the need for rare disease diagnostics to be made a public health priority. Considering there are around 7000 clinically defined rare diseases this translates into 3.5-5.9% of the worldwide population being affected at any point in time, equivalent to 300 million people. Even then, this is regarded as conservative as the figure calculations did not take into account rare cancers, rare disease caused by rare bacterial or viral infectious diseases and poisonings.4 As it stands, however, 300 million vastly exceeds the global figure of 18.1 million assigned to new cancer cases worldwide in 2022.5
To illustrate the relevance of rare disease screening, of those clinically defined, 72% are genetic, and 70% of those start in childhood.4 Therefore having, accurate, sensitive testing methods with high throughput capabilities and flexibility is key.
Next generation sequencing (NGS) is extensively used for genetic testing as nucleotides in hundreds and thousands of genes, in targeted regions or the whole genome, can be determined in a matter of days. Subsequent, analysis of the resulting data leads to the revelation of disease-causing single nucleotide variants (SNVs), insertion/deletions (INDELs) and copy number variations (CNV). In this blog, we will look into the three ways NGS is used to screen for rare disease variants, highlighting the importance of including non-coding regions in rare disease diagnostics.
The application of NGS in rare disease variant detection
Genomic analysis offers a distinct advantage over other technologies, like proteomics and metabolomics. Unlike the proteome, which dynamically changes across cells and over time, the genome remains largely consistent making it a reliable reference for identifying genetic variation.
Whole genome sequencing (WGS) is considered the gold standard for broadly questioning complex genomic issues, but it has limitations. While it captures the entire genome, including both coding and non-coding regions, the all-encompassing nature of WGS may not be essential in every scenario. Notably, the extensive data generated requires deep sequencing and significant computational analysis, leading to high costs and potentially unnecessary information overload.
In the context of rare disease screening, especially when diagnostic biomarkers have been identified, opting for WGS may be excessive and alternative NGS methods can be more cost-effective and efficient for specific diagnostic purposes. Therefore, the choice of technology should be tailored to the specific needs of each clinical investigation.
What are the alternatives to WGS?
- Whole exome sequencing (WES) is a more cost-effective approach than WGS as it focuses on the protein-coding region covering approximately only 2% of the whole genome.9 The limiting factor here is that non-coding regions are excluded so additional tests, or WGS, are needed to analyze them adding time and cost pressures to testing laboratories
- Targeted sequencing is the most cost-effective approach as only your selected gene regions require analysis. By designing panels to cover specific variants, genes of interest from both coding and non-coding regions can be accommodated. A targeted approach is therefore viable when definitive molecular diagnosis isn’t possible from WES. An additional benefit is flexibility, as targets can be added to panels as new variants are added to clinical test directories
While WES plays a crucial role in diagnosing rare Mendelian diseases, capturing 30-50% of cases, it is limited to analysis of the protein-coding regions.10 However, it is widely recognized that the vast non-coding regions harbor critical regulatory elements, and structural variations, that hold clues to disease mechanisms. Therefore, relying solely on WES will miss identifying disease-causing variants.7
Finding the right balance is key. Instead of resorting to costly WGS, targeted approaches can bridge the gap to strategically investigate specific non-coding regions. With this in mind alongside comprehensive WES, we can gain deeper insights into causative reasons for disease.
Getting the best of both worlds
Diagnosing rare disease presents a complex puzzle. While WES is a powerful genomics tool, it only analyzes protein-coding regions, leaving the vast non-coding landscape unexplored.
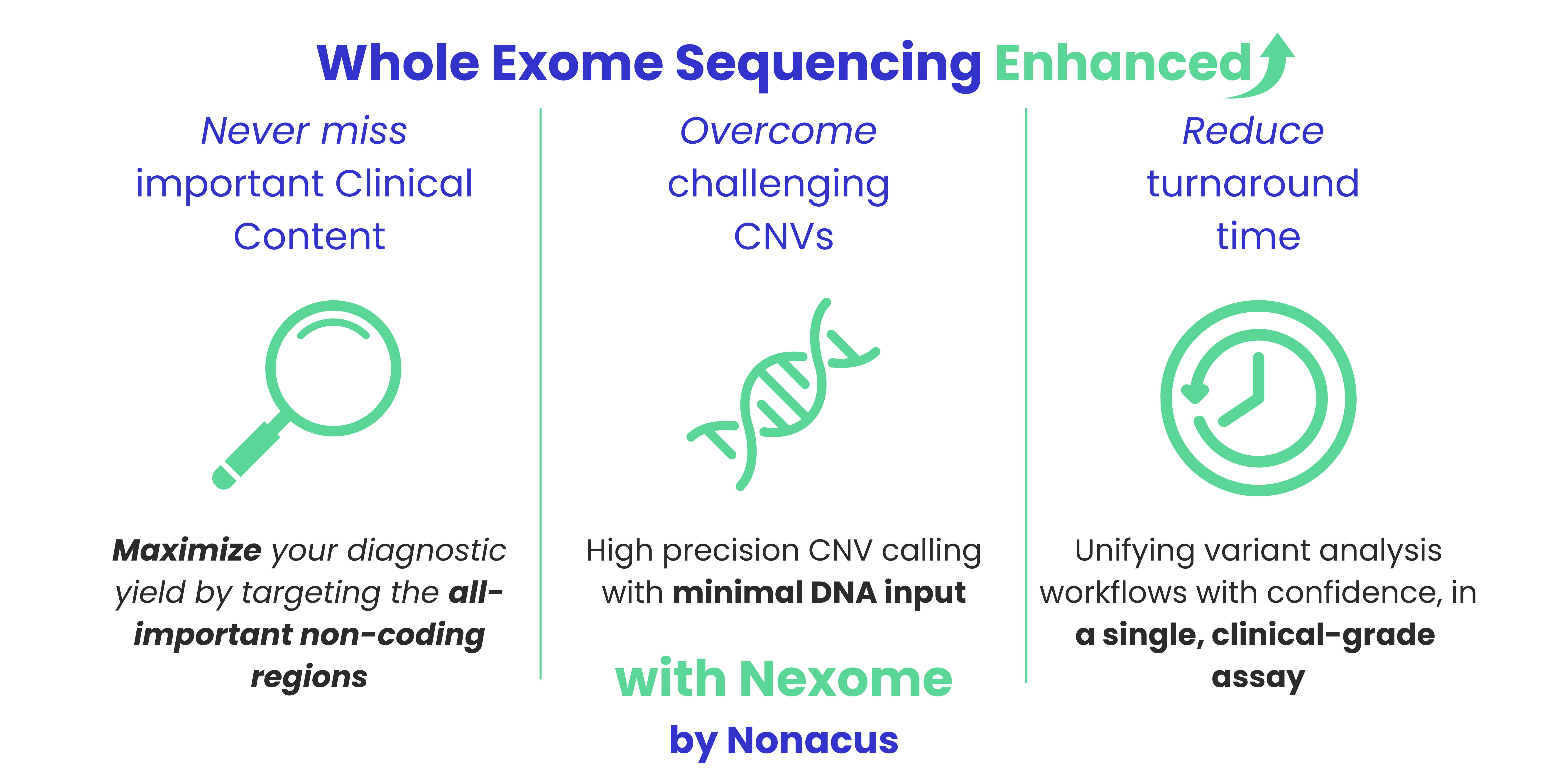
Cell3™ Target: Nexome bridges this gap as an innovative NGS solution merging comprehensive WES with targeted key non-coding regions, in one workflow. This robust design, delivering SNV, INDEL and CNV detection, delivers a broader and deeper view of the genetic landscape, with additional pharmacogenomic (PGx) markers for drug response prediction.14
Do you have challenging sample types?
Don’t be excluded if your DNA is highly fragmented, or low in concentration, or both. Cell3 Target: Nexome is compatible with all types of DNA, is automatable and requires as little as 1 ng DNA. Maximizing the scope of DNA input means you can collect the most suitable sample type from across your patient group.
- Genomic DNA (gDNA) from fresh frozen tissue, blood and saliva
- FFPE gDNA from wax tissue-embedded scrolls
- Cell-free DNA (cfDNA) extracted from plasma, serum, saliva, cerebrospinal fluid and amniotic fluid
- Sensitive enough to detect variants in cell-free fetal DNA (cffDNA)
Conclusion
NGS is revolutionizing rare disease diagnosis by uncovering crucial variants in previously hidden non-coding regions, alongside traditional WES or WGS. With this in mind the content combination of Cell3 Target: Nexome unlocks the potential for earlier diagnosis, targeted treatment strategies to ultimately improve patient outcomes.
References
- Abozaid GM, Kerr K, McKnight A, Al-Omar HA. Criteria to define rare diseases and orphan drugs: a systematic review protocol. BMJ Open. 2022;12(7):e062126. doi:10.1136/bmjopen-2022-062126
- Rare Disease Database. https://rarediseases.org/rare-diseases/. Accessed 8 February, 2024
- European Commission. Rare Diseases. https://research-and-innovation.ec.europa.eu/research-area/health/rare-diseases_en. Accessed 8 February, 2024.
- Nguengang Wakap S, Lambert DM, Olry A, Rodwell C, Gueydan C, Lanneau V, et al. Estimating cumulative point prevalence of rare diseases: analysis of the Orphanet database. European Journal of Human Genetics. 2020 Feb;28(2):165-73.
- Cancer statistics. https://www.cancerresearchuk.org/health-professional/cancer-statistics/worldwide-cancer. Accessed 22 February 2024
- Marwaha S, Knowles, JW, & Ashley EA. (2022). A guide for the diagnosis of rare and undiagnosed disease: beyond the exome. Genome medicine. 2022;14(1):1-22.
- Gloss BS & Dinger ME. Realizing the significance of noncoding functionality in clinical genomics. Experimental & molecular medicine. 2018;50(8):1-8.
- National Human Genome Research Institute. https://www.genome.gov/about-genomics/educational-resources/fact-sheets/human-genomic-variation. Accessed February 8, 2024.
- Oxford Health NHS Foundation Trust. https://www.oxfordhealth.nhs.uk/cit/resources/genetic-rare-disorders/. Accessed February 8, 2024.
- Frésard L, Montgomery SB. Diagnosing rare diseases after the exome. Molecular Case Studies. 2018 Dec 1;4(6):a003392.
- Smedley D, Schubach M., Jacobsen JO, Köhler S, et al. A whole-genome analysis framework for effective identification of pathogenic regulatory variants in Mendelian disease. The American Journal of Human Genetics. 2016;99(3):595-606.
- Landrum M.J, Lee JM, Benson M, Brown G R, Chao, C, Chitipiralla, S. et al. ClinVar: improving access to variant interpretations and supporting evidence. Nucleic acids research. 2018;46(D1), D1062-D1067.
- McKusick, V. (2009). Online Mendelian Inheritance in Man, OMIM™. McKusick-Nathans Institute for Genetic Medicine, Johns Hopkins University (Baltimore, MD) and National Center for Biotechnology Information, National Library of Medicine (Bethesda, MD), 2000. World Wide Web URL: https://omim. org.
- Cell3 Target: Nexome –a clinically enhanced exome panel. Accessed February 8, 2024.